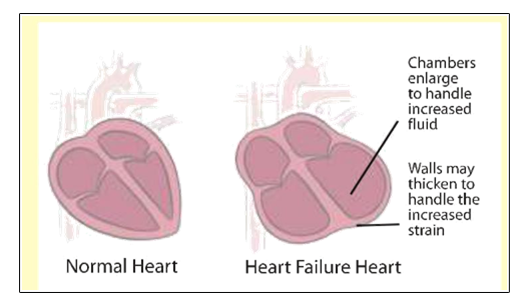
Heart failure is a condition characterized by reduced pumping ability of the heart. As a result, the heart cannot pump enough blood to fulfill the nutritional requirements of the body. It is the end result of various cardiac disorders such as a heart attack, untreated high blood pressure, coronary artery disease or incessant tachycardia.
As a result, fluid may build up in the lungs, legs and in other tissues throughout the body leading to shortness of breath, reduced exercise capacity and breathlessness at night. The term “Congestive Heart Failure” is sometimes used to describe the condition.
One of the ways heart failure can be identified is to measure the percentage of blood that is pumped out of the heart during each beat. This percentage is called the ejection fraction. In a healthy heart, 50-70% of the blood is pumped out during each beat. Patients with heart failure usually have a reduced ejection fraction, often less than 35%.
Your symptoms will help the doctor classify the severity of your failure and monitor the response to drug and device therapy.

Heart failure can develop for many reasons. There is no single cause and sometimes the cause is unknown. Some of the common causes of heart failure are :
Coronary artery disease Heart attack
Uncontrolled high blood pressure
Heart valve problems
Infection of the heart
Long-term alcohol abuse
Heart problems you are born with
What Can I Do?
Although heart failure cannot be cured, it can be managed effectively. Your treatment plan may include medicines, surgery, special pacemakers or a combination of these. You can also do a lot to manage your health by following your treatment plan, watching your weight, eating a low-sodium diet, exercising and staying connected with family and friends. With good care, you can live a fulfilling and meaningful life.
Therapies for Heart Failure
Devices :
A Medtronic heart failure pacemaker is one part of an overall heart failure treatment plan. Devices used for heart failure include :
A heart failure pacemaker – Helps coordinate the heart’s pumping action and improve blood flow. It can also speed up a heart that is beating too slowly. Because the pacemaker helps”synchronize”the heart, it is sometime called cardiac resynchronization therapy.
A combination heart failure pacemaker/defibrillator – Resets a heart that’s beating dangerously fast in addition to synchronizing your heart beat. Your doctor may refer to this as an ICD (Implantable Cardioverter Defibrillator).
In addition to a heart failure pacemaker, your doctor may treat your heart failure in other ways. These include the medicines, lifestyle changes and surgical procedures listed below. You should carefully follow your doctor’s advice regarding all of these therapies.
Heart Failure Medicines
ACE (angiotensin-converting enzyme) inhibitors
Beta-blockers
ARBS (angiotensin receptor blockers)
Diuretics (water pills)
Aldosterone antagonists
Blood thinners
Digoxin
Self-care
Taking your medicines as described
Following a low-sodium diet
Monitoring your weight daily
Exercising
Quitting smoking
Losing weight
Reducing or ceasing alcohol consumption
Surgery
Heart valve repair or replacement
Left-ventricular assist device
Heart transplant

A heart failure pacemaker continuously monitors your heart 24 hours a day. If the device detects a problem, it sends out small electrical signals you can’t feel to correct your heart’s pumping action. These signals travel over three small-insulated wires that connect the device to your heart.
Heart Failure Pace-Maker
The heart failure pacemakers are small about the size of a pocket watch or smaller. The battery and computer circuitry needed to correct your heart rhythm are contained in the device. Small-insulated wires connect the device to your heart.
Talk to your doctor about the differences between a heart failure pacemaker with or without defibrillator and about which type may be right for you.

In normal individuals, there is rapid activation of the lower chambers (ventricles) which causes synchronized and efficient pumping of the heart. In some patients with heart failure, there is a delayed activation of the ventricles which leads to dyssynchronous and ineffective contraction. CRT causes simultaneous pacing of the septal and lateral walls of the left ventricle which restores ventricular synchrony and improves cardiac efficiency. CRT has been shown to improve symptoms of heart failure, reduce chances of hospitalization due to heart failure and increase long-term survival of patients.
Benefits of Cardiac Resynchronization Therapy
Many people experience dramatic improvements in their quality of life and in their heart failure symptoms after receiving a Medtronic heart failure pacemaker i.e. cardiac resynchronization therapy. They have more energy and can do things they never thought they would do again.
Not everyone responds to cardiac resynchronization therapy in the same way, and your experience may vary. But research has shown that cardiac resynchronization therapy reduces the chance people with heart failure will have to go to the hospital. It can also reverse some of the changes in the heart’s shape and function caused during heart failure.
During the implant:
The procedure is performed under local anesthesia and patients are awake throughout the procedure. Your doctor will make a small incision in the upper chest below the collar bone and guide three thin insulated lead wires through a vein and into the heart. The procedure does not require open-heart surgery.
The lead wires are connected to the device (pulse generator) and the doctor will program the device settings. Finally, the device will be inserted beneath the skin and the incision in your chest will be closed. Most people stay in the hospital overnight and go home within a couple of days.
Implant procedure
2-inch incision below the collar bone
3 insulated wires (leads) guided through vein and into heart
Lead parameters are checked and leads sutured to the underlying muscle
Leads connected to device
Device programmed and tested
Device inserted beneath the skin
Incision closed
After the procedure
Following the implant, people will typically stay overnight in the hospital and go home within a couple of days. Your doctor will provide you with specific instructions on how to care for your incision and information on signs and symptoms that may require further medical attention. Usually, you can expect to return to your everyday activities a few days after the implant procedure. If you have any questions, ask your doctor.
Follow-up care
After the implant, the doctor who implanted your heart pacemaker will work together with your heart failure doctor to manage your care. You should continue to take the prescribed heart-failure medications after the procedure. It is important to keep appointments with both specialists and to follow their recommended daily care to ensure the best possible results.
You may feel more energetic and ready to resume some of your normal activities shortly after receiving a heart failure pacemaker. The goal is for you to lead a more normal life as soon as possible.
The device should not affect your ability to do most everyday activities around the house. You should also be able to enjoy your hobbies, return to work, participate in sexual activity and travel.
As you return to your old activities or start new ones, you may have questions about how your activities will impact the function of your heart failure pacemaker. The section below provides general information on a number of frequently asked questions.
Cellular Telephones
Yes. But to avoid any interference, don’t put a cell phone in the breast pocket near your heart failure pacemaker, and when talking on the phone, use the ear opposite of your device.
Driving
It depends on the state where you live. Most people with a Medtronic heart failure pacemaker are able to resume driving based on the laws and insurance regulations in their state and on their doctor’s recommendation.
Travel
Most people with a heart failure pacemaker can travel without taking special precautions. Your doctor or nurse can provide instructions on clearing airport security.
Follow-up and Replacement
The doctor who implanted your device will schedule regular follow-up appointments to check up on your device. If your doctor finds that the battery is low, he or she will discuss a replacement procedure. Because the battery inside the pulse generator cannot be recharged, the device must be replaced, which typically occurs within 7 years of initial implant. Only the pulse generator is replaced and not the lead wires.
The following questions have been prepared to help guide discussion with your physician regarding heart failure pacemakers. These questions are intended only as a starting point in your dialogue with your doctor about the various options available today to treat heart failure.
Do you think a heart failure pacemakers could help me?
If so how? If not, why not?
What is the difference between a heart failure pace-maker with or without a defibrillators?
Do you currently have other patients who have received a heart failure pacemaker? If so, how has it helped them?
Have any patients gotten worse?
If I get a heart failure pacemaker, willl still take medicines for my heart failure?
If this treatment option is prescribed for me, who will put in the device?
What are the risks associated with the implants?
How often will my heart failure pacemaker need to be checked and by whom?
When can I resume normal activities after my heart failure pacemaker is implanted?
What’s the next step in considered a heart failure pacemaker as a treatment option for my heart failure?
* Please note that physician prescribe heart failure pacemaker only for patients with specific heart failure signs and symptoms. In clinical trials, not all patients experience positive results with heart failure pacemakers. Please consult with your physician to determine if you are a candidate for a heart failure pacemaker. Your physician should discuss all potential benefits and risks with you.
Watch for physical signs that may indicate that your pacemaker & medical condition need to be checked. Call your doctor immediately if any of these symptoms occur :
1) Difficulty in breathing, dizziness, or fainting spells
2) Swelling of the legs, ankles, arms, or wrists
3) Chest pain or prolonged hiccups
4) Fever along with redness, swelling, or drainage at the incision site
Consult your doctor if you experience unusual heart rate increases or palpitations during sleep or other inappropriate times.
Visit your doctor or pacemaker clinic regularly for follow-up visits and other check-ups. Follow your doctor’s schedule for telephone follow-up of your pacemaker if this has been prescribed for you.
Follow your doctor’s instructions concerning diet, medications, and physical activity. Tell your doctor if you plan to change activity levels or lifestyles, take a trip or change you address.
Tell any new doctor, dentist, or other health professional that you have a pacemaker. If you have a rate responsive or dual chamber pacemaker, tell them the pacemaker is designed to change rates. Make sure your doctor knows what type of pacemaker you have before any medical or surgical procedure is undertaken.
Consult with your doctor if you have questions related to your heart, your condition, or your pacemaker.
Carry your identification card at all times.