Cardiac electrophysiology is a subspecialty of cardiology that deals with diagnosis and treatment of heart rhythm disorders (arrhythmias). Symptoms of arrhythmias include palpitations, dizziness, syncope, and breathlessness. Heart rhythm disorders are broadly classified into two types: tachyarrhythmias and bradyarrhythmias. Normal resting heart rate varies from 60 to 100 beats per minute (bpm). When an arrhythmia is associated with a heart rate more than 100bpm, it is called as tachyarrhythmia. On the contrary, heart rate < 60bpm associated with symptoms such as dizziness and syncope is referred as bradyarrhythmia.

A cardiologist who has undergone specialized training in treating heart rhythm disorders.
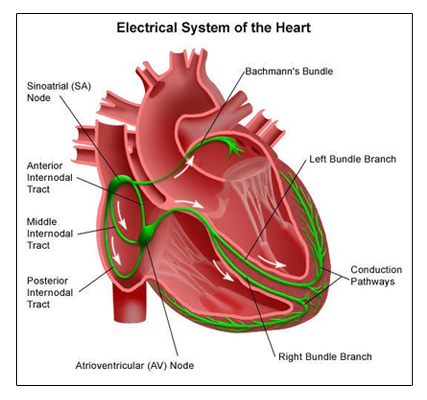
The heart is a muscular organ that pumps oxygen-rich blood to all the tissues of the body. It has two upper chambers, the right and left atria, and two lower chambers, the right and left ventricles. The upper chambers (atria) receive blood from different parts of the body and the lungs. The lower chambers (ventricles) pump blood to various parts of the body and the lungs. Normally, the heart’s pumping is initiated by electrical pulses produced by the Sinoatrial (SA) node, heart’s natural pacemaker, located in the right atrium. Electrical impulses generated by the SA node travels through the atria, stimulating the atria to contract and pump blood into the ventricles. Impulses from the atria are then conducted to the ventricles through the Atrioventricular (AV) node and the bundle of His, which is the only electrical connection between the atria and the ventricles. The bundle of His bifurcates into the right bundle branch which activates the right ventricle and the left bundle branch which stimulates the left ventricle. Normally, there is a delay in conduction at the AV node so that the electrical impulses reach the ventricles only after the atria have contracted. This phenomenon of conduction delay ensures AV synchrony.
Under resting conditions, the SA node fires at a rate of 60 to 100 beats per minute. The heart rate increases proportionately during physical activity, which is modulated by impulses from the brain. During strenuous exertion, the heart rate can increase to >150 beats per minute to meet the high nutritional requirements of the exercising muscles. On the contrary, heart rate may be < 60 beats per minute during sleep, which is normal.
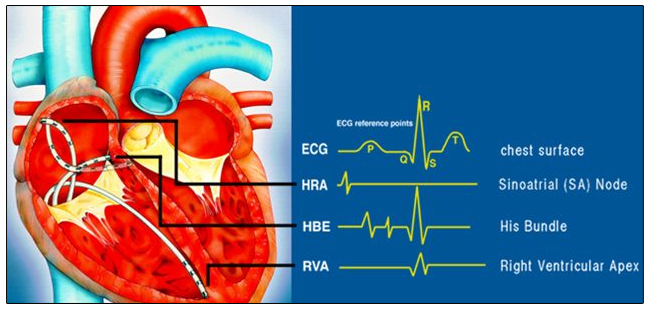
It is a minimally invasive procedure in which multiple catheters are strategically positioned in different chambers of the heart to record the activation pattern of electrical impulses in the heart. In this way, the electrophysiologist will precisely map the abnormal focus or circuit that is responsible for causing the arrhythmia. Mapping catheters are inserted via the blood vessels of the groin and the neck.
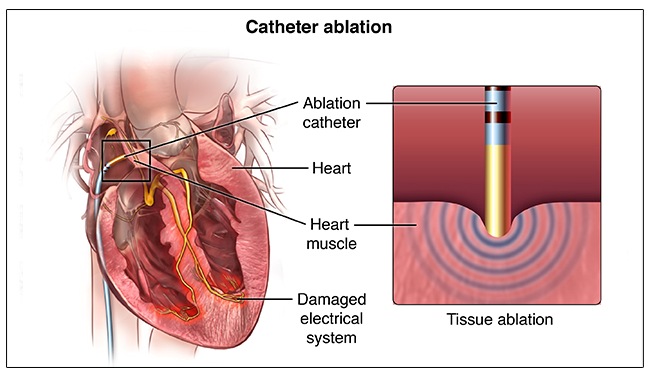
It is a procedure in which the abnormal focus delineated during the electrophysiological study is ablated (neutralized) by delivering radiofrequency or cryothermal energy through a specially designed catheter introduced through the vascular system of the groin.
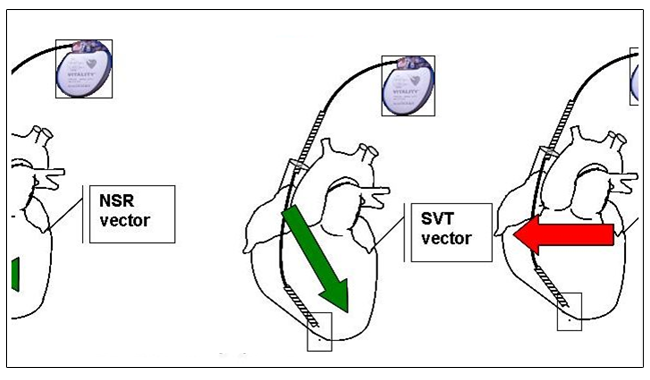
Tachyarrhythmias are classified as supraventricular tachycardia (SVT) and ventricular tachycardia (VT). When the abnormal focus or circuit causing arrhythmia is located at least partially in the atria (upper chambers), it is termed as SVT. When the abnormal focus or circuit is located entirely within the ventricles (lower chambers), it is frequently life-threatening and is termed as VT. Atrial fibrillation is the most common tachyarrhythmia in which there is irregular, chaotic, and continuous activation of the atria that can lead to blood clots, stroke, and heart failure.
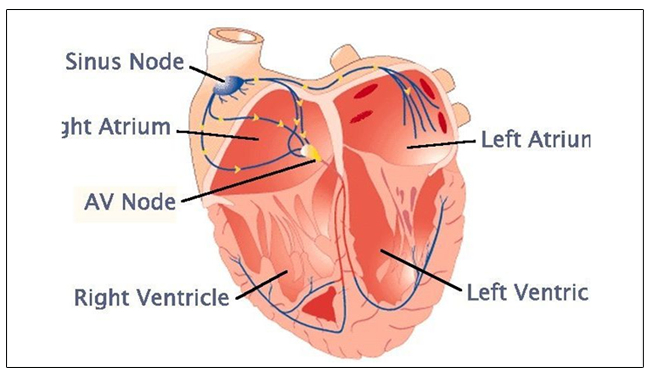
Bradyarrhythmias may be divided into disorders of impulse formation and disorders of impulse conduction. The sinoatrial node is the natural pacemaker of the heart located in the right atrium. It is responsible for generating normal electrical impulses at a rate of 60-100 bpm. Sinus nodal dysfunction leading to an abnormal impulse formation and low heart rate is referred as sick sinus syndrome. When electrical impulses from the atria fail to conduct to the ventricles, it is termed as atrioventricular block.
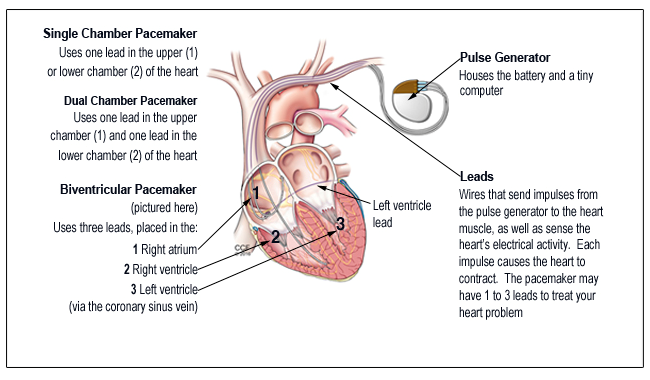
A permanent pacemaker is a small device that monitors the heart rhythm and paces the heart when the intrinsic rate is abnormally low. A conventional pacemaker comprisesa pulse generator that is implanted underneath the skin below the collar bone and pacing leads that are positioned inside the cardiac chambers. The newer leadless pacemaker consists of a pulse generator that is directly implanted into the cardiac chamber without any intervening leads.
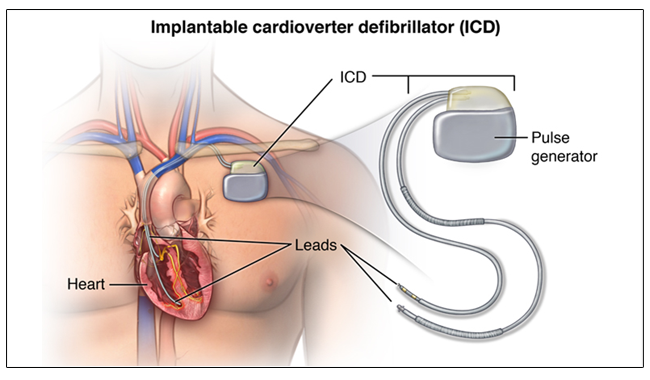
It is an implantable device, similar but more sophisticated than a pacemaker, which continuously monitors the heart rhythm, and delivers treatment in the presence of life-threatening arrhythmias such as ventricular tachycardia and ventricular fibrillation. ICDs have been shown to reduce the long-term risk of sudden cardiac death and overall mortality.
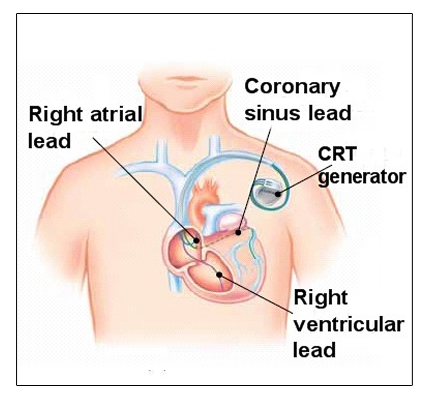
In patients with heart failure and left bundle branch block, there is a dyssynchronous contraction of the left ventricular septum and lateral wall leading to a reduced left ventricular ejection fraction. CRT restores synchrony by simultaneously pacing the septum and lateral wall and thereby augments cardiac efficiency. In the long term, CRT has been shown to increase left ventricular ejection fraction as well as reduce mortality and heart failure hospitalizations.