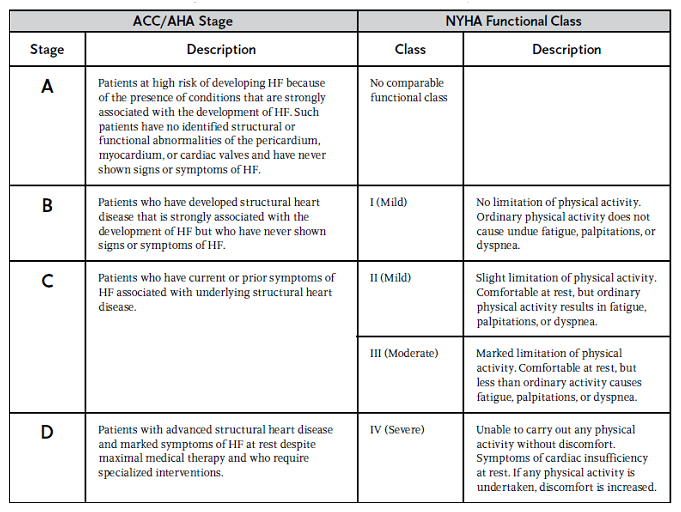
Heart failure (HF) is a progressive syndrome with many underlying causes. Clinically, it is perhaps better defined as ventricular dysfunction that limits a patient’s ability to perform routine activities of daily living. Formally, based on the American College of Cardiology (ACC)/American Heart Association (AHA) 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult, HF is defined as “a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood.” Heart failure alone accounts for over one million hospital admissions each year.
The most common cause of heart failure is coronary artery disease (CAD). CAD blocks the flow of blood to the arteries and leads to ischemia or myocardial infarction, which in turn weakens the myocardium and reduces its contractile force. Cardiomyopathies are disorders of the myocardium.
HF is caused by the loss of a critical quantity of functioning myocardial cells after injury to the heart due to (most to least common):
Ischemic heart disease
Hypertension
Idiopathic cardiomyopathy
Infections (e.g., viral myocarditis, Chagas’ disease)
Toxins (e.g., alcohol or cytotoxic drugs)
Valvular disease
Prolonged arrhythmias
Ischemia weakens the myocardium and reduces its contractile force, and therefore leads primarily to systolic dysfunction. Chronic hypertension forces the myocardium to work harder to overcome increased vascular resistance (after load). The extra work thickens the myocardium and prevents full relaxation during ventricular filling, and therefore leads to diastolic dysfunction.
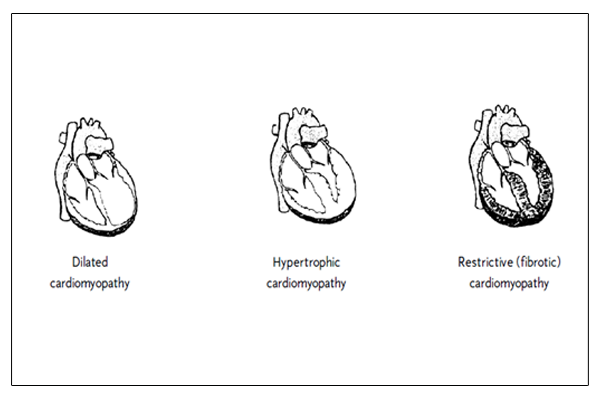
There are three types of Cardiomyopathy which can happen which in turn cause Heart Failure :
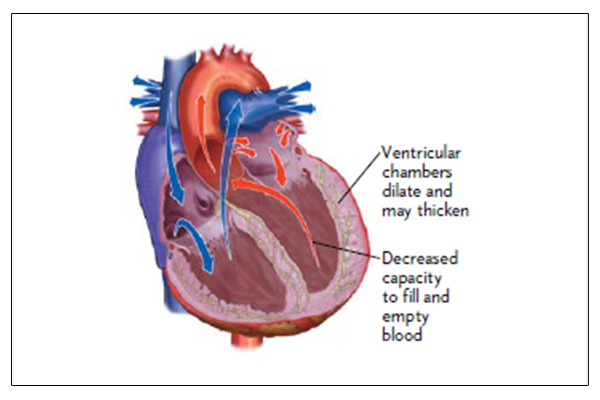
Dilated cardiomyopathy is enlargement of the heart chambers, especially the ventricles, due to a weak myocardium. It increases heart wall stress and reduces blood flow to the myocardium, decreasing its ability to contract effectively (systolic dysfunction).
Hypertrophic cardiomyopathy is a thick or bulky myocardium that initially causes abnormal diastolic relaxation. The added bulk limits ventricular compliance (ability to stretch) during diastolic filling. With time, systolic dysfunction often develops.
Restrictive cardiomyopathy is a stiff (fibrotic) myocardium that does not relax effectively. It causes poor diastolic filling.
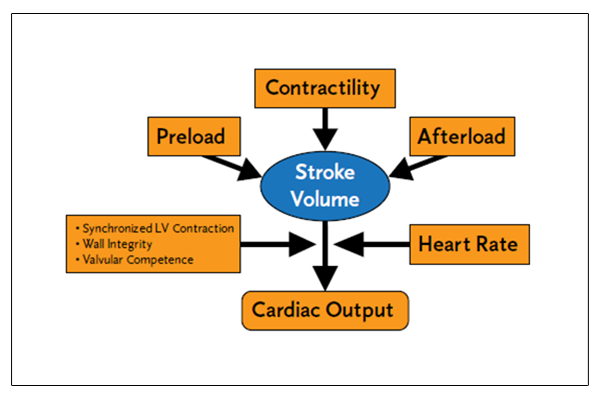
Cardiac output is equal to the heart rate multiplied by the Stroke volume (CO = HR × SV). The stroke volume is the amount of blood the heart ejects per heartbeat. Normal stroke volume is 60-100 milliliters; cardiac output is normally 4-8 liters per minute.
Stroke volume is affected by preload, after-load, and contractility.
Preload is the amount of myocardial stretch at the end of diastole.
After - load is the resistance that needs to be overcome for the heart to eject the blood.
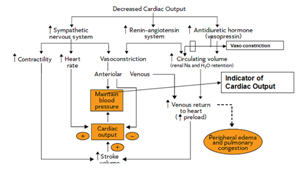
When heart failure patient experiences decreased cardiac output, the body tries to compensate and bring it back to normal.
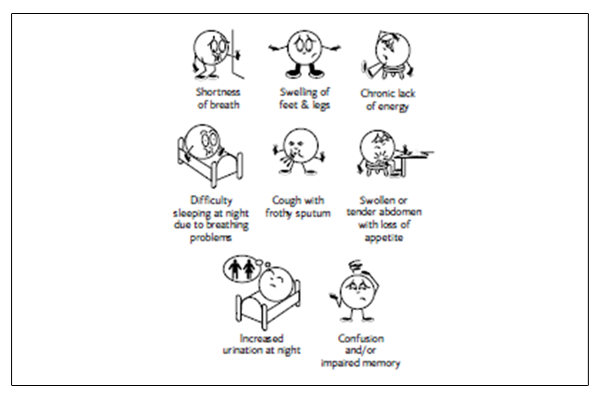
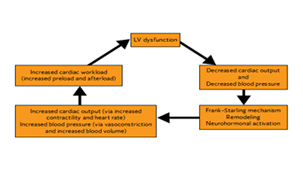
Left ventricular dysfunction moves from a compensated to a decompensated state. Decompensated means the heart can no longer compensate for insufficient cardiac output. As a result some HF symptoms occur..
Many factors can cause patients to move between compensated and decompensated heart failure. Several compensatory mechanisms are activated in HF to buffer the fall in cardiac output and help maintain sufficient blood pressure in order to perfuse vital organs.
Mean Arterial BP = (CO* Peripheral Resistance) is the direct Measure of Reduced CO.
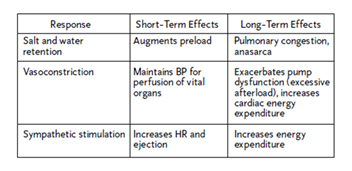
The main compensatory mechanisms that are triggered with HF are:
The Frank-Starling mechanism
Cardiac remodeling
Activation of neurohormonal systems
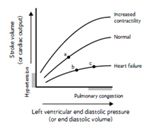
1. The Frank-Starling mechanism attempts to keep right and left cardiac outputs balanced (to a point). The law states that the strength of ventricular contraction Varies directly with preload. Thus within physiologic limits, the more the normal ventricle is stretched during diastole, the stronger the heart will contract and the greater the volume of blood ejected during systole.
Example : If the right ventricle pumps a little more blood than the left, the volume of blood flowing from right heart to left heart increases (preload). This builds pressure in the LV and enables it to stretch and contract more forcefully on the next beat (contractility), thus ejecting more blood and keeping up with the right side output.
In heart failure, as the myocardium weakens, more preload pressure is needed to achieve the same cardiac output. At a given point, the stretch-contractility relationship begins to fail – that is, increased stretch no longer leads to increased cardiac output. At this point, LV dysfunction moves to a decompensated state.
2. Heart failure is a progressive disease, and the chronic hemodynamic stresses imparted on the failing heart eventually lead to alterations in the heart’s size, shape, structure, and function. This process is known as remodeling. Initially, the changes that occur with remodeling can be considered compensatory.
For example, the dysfunctioning heart has a compromised stroke volume; thus, one adaptive mechanism to maintain stroke volume is to enlarge the ventricular volume (ventriculardilatation) so that a greater stroke volume results from a reduced ejection fraction.
The progressive nature of remodeling that occurs in the failing heart eventually becomes detrimental. Continued hypertrophy and dilatation of the ventricle inevitably lead to increasing ventricular wall stress, and ongoing fibrosis and the damaged myocardium increasingly impair contractility. This remodeling is believed to cause an increase in cell death (apoptosis).
3. Compensatory Neurohormonal Stimulation includes the natriuretic peptides. The natriuretic peptides – ANP, BNP, and CNP – are vasodilating neurohormones. As such, they play animportant role in counter-regulating the vasoconstricting effects of other neurohormones.
Its level seems to correlate with the amount of shortness of breath and left ventricular volume and pressure. For this reason, the level of BNP may be the first “white count” for heart failure.
The natriuretic peptides act directly on blood vessels to cause vasodilatation. They also have natriuretic (salt-excreting) and diuretic (water-excreting) effects because of their ability to inhibit the secretion of renin, aldosterone, and vasopressin. The degree of elevation of natriuretic levels is directly related to mortality.
Vicious Cycle of Heart Failure
Neurohormonal Responses to Impaired Cardiac Performance
Initially Adaptive, Deleterious if Sustained
Systolic: Impaired contractility / ejection.
Approximately two-thirds of heart failure patients have systolic dysfunction.
Diastolic: Impaired filling/relaxation
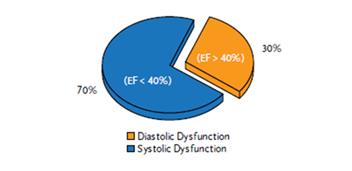
As the above suggest, there are many causes of heart failure. Some diseases, however, tend to more adversely affect the heart’s systolic function (ventricular contraction/ejection), while others tend to more adversely affect diastolic function (ventricular filling/relaxation). This provides a useful way of classifying heart failure from a hemodynamic standpoint. Most patients who have systolic dysfunction also have a component of diastolic dysfunction.
Approximately two-thirds of heart failure patients exhibit systolic dysfunction. In systolic dysfunction, the ventricular myocardium cannot contract with enough force to eject sufficient blood into circulation. Normally about 55% to 65% of blood is ejected from the ventricles per contraction (ejection fraction, or EF).
Patients with LV systolic dysfunction typically have an EF of 40% or less. In diastolic dysfunction, a lower total volume of blood is ejected even though the EF may be normal. Filling pressures are higher than normal because of poor ventricular compliance.
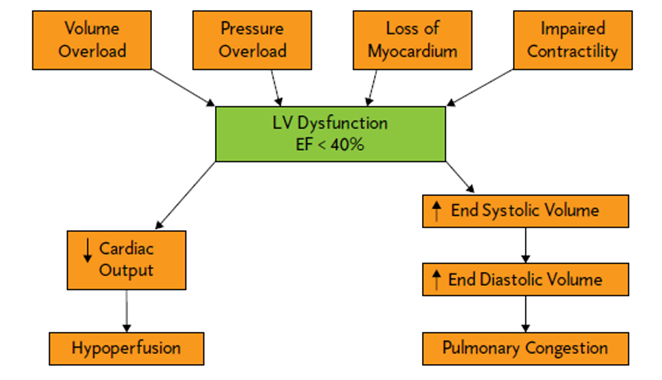
Left Ventricular dysfunction causes decreased cardiac output, which can cause hypo-perfusion of the body’s organs. In addition, there can be an increase in the amount of blood left in the ventricle when the heart squeezes, and therefore, both end systolic and end diastolic volumes are subsequently increased. This increase in volume can lead to pulmonary congestion and shortness of breath.
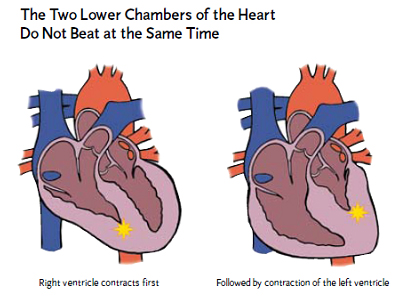
The distortions in the heart’s anatomy (cardiac remodeling) that occur with chronic heart failure often have significant adverse effects on the electromechanical function of the heart. These adverse electromechanical effects, which include intraventricular and interventricular conduction delays, left ventricular dilation, dyskinetic septal wall motion, and mitral valve regurgitation, can be readily evaluated by echocardiogram.
Studies have shown that up to 50% of patients with systolic heart failure have prolongation of the PR interval and intraventricular conduction defects, such as left bundle branch block, that lead to a loss of coordinated ventricular contraction. This loss of coordinated ventricular contraction, or ventricular dyssynchrony, has been associated with diminished cardiac function and increased mortality.
Three major types of drugs are used for heart failure patients :
Diuretics – Most patients with heart failure require a diuretic to relieve fluid retention. In addition to rapidly decreasing symptoms such as pulmonary congestion and peripheral edema, diuretics improve exercise tolerance and facilitate the use of other drugs indicated for heart failure.
ACE inhibitors or ARBs – Angiotensin-converting enzyme (ACE) inhibitors block the conversion of angiotensin I to angiotensin II, thereby reducing circulating levels of angiotensin II. Recall that in HF, angiotensin II has a number of adverse effects, including vasoconstriction, salt and water retention, and activation of the SNS.
Beta blockers – which were long thought to be contraindicated in HF because of their negative effects on myocardial contractility, are now considered an important part of HF care. Long-term treatment with beta blockers has been shown to have a number of positive effects, including improving the symptomatic and clinical status of patients with HF, reducing ventricular arrythmias, and reducing mortality.
Digoxin – is a positive inotropic agent that has been shown to improve symptoms, quality of life, and exercise tolerance in patients with mild to moderate HF; however, it has not been shown to reduce mortality from HF.
Cytokines – are small protein molecules that decrease the strength of ventricular contraction, and thus are known as negative inotropes.
Aldosterone levels are elevated in patients with chronic heart failure. Because elevated levels of circulating aldosterone promotes salt and water retention by the kidneys and exerts adverse effects on the structure and function of the heart, agents that antagonize aldosterone have emerged as a relatively new and important way to treat severe, chronic HF. Spironolactone is the most widely used aldosterone antagonist.
In people diagnosed with Congestive Heart Failure (CHF), SCA occurs at six to nine times the rate of general population.
About one - half of all deaths in heart failure patients are as sudden due to arrhythmias.