The normal heart is about the size of your clenched fist, small for the amount of work it does. This special muscle pumps about five quarts (4.7 liters) of blood throughout your body each minute, or 75 gallons (284 liters) every hour. Its steady, rhythmic pumping sends oxygen-rich blood throughout the body.
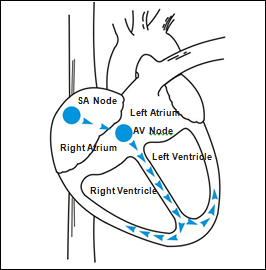
Your heart has two upper chambers– the atria – and two lower chambers– the ventricles. The atria pump blood into the ventricles. The right ventricle then pumps blood to the lungs while the left ventricle pumps blood to all your body’s organs. Normally, your heart’s pumping is controlled by steady electrical signals produced by your heart’s “natural pacemaker,” the sinoatrial (SA) node. The signals travel through the atria to a junction in the middle of the heart, the atrioventricular (AV) node. The signals then continue throughout the ventricles. The heart then rests until the next pulse begins the cycle over again.
These signals keep your heart beating steadily and rhythmically at about 60 to 80 beats per minute at rest and higher as your activity level increases.
The heart’s electrical system may develop a problem that prevents the electrical signals from reaching the pumping chambers regularly. The problem could also cause the signals to be generated erratically or too quickly. When the signals are generated too quickly, the heart beats too fast. This rhythm disorder is called a tachy-arrhythmia. Tachyarrhythmias may result from heart disease such as coronary artery disease, a heart attack, or heart muscle disease (cardiomyopathy).
When your heart beats too quickly and the impulses start in the lower chambers, the tachyarrhythmia is called a ventricular tachycardia (VT).
When your heart goes into VT, it may not pump blood as efficiently as it does during a normal rhythm. Rapid contractions prevent it from filling adequately with blood between beats. Less blood reaches your brain. During VT you may feel your heart pound or feel faint or dizzy. You may even pass out. VT can be dangerous, even life-threatening, if not properly treated.
When a ventricular tachyarrhythmia becomes unstable and irregular, it is called ventricular fibrillation (VF). During VF, your heart beats in a disorganized manner. It quivers. No blood is pumped and your body is quickly starved of oxygen. If your heart goes into VF, you usually pass out within a few seconds. Your heart’s electrical activity may become so erratic that your heart no longer pumps blood at all, a situation commonly called a cardiac arrest.
Cardiac arrest usually occurs without warning. Emergency medical teams try to revive people from cardiac arrest by using the paddles of machines called external defibrillators to apply strong defibrillation shocks to the chest. These shocks pass through to the heart, stop the erratic electrical activity, and allow the heart to return to a more regular rhythm.
Unfortunately, emergency teams and their external defibrillators are rarely available in the first moments of cardiac arrest. Your Medtronic implantable cardioverter defibrillator (ICD) contains an internal defibrillator and pacemaker. The defibrillator acts as an automatic “watch dog” during those first crucial seconds. When your heart goes into a tachyarrhythmia, the defibrillator paces or shocks your heart out of VT or VF.
Sometimes the heart beats too slow to meet the body’s demands. This condition is called bradycardia. Symptoms of bradycardia may include dizziness, extreme fatigue, shortness of breath, or fainting spells.
If your heart beats too slow or you experience bradycardia, the pacemaker contained in your ICD restores regular electrical impulses to your heart, allowing it to pump more blood and relieve the symptoms.
Bradycardia is usually caused by the SA node not working properly or by a condition called heart block.
“ICD” is an abbreviation for Implantable Cardioverter Defibrillator, An ICD delivers therapies to treat heart rhythm disorders, such as VT and VF, The ICD is implanted inside your body and works automatically.
Your medical condition determines the type of ICD that you receive. Your doctor has recommended the particular model of ICD that will best treat your rhythm disorder. Each model varies somewhat in its size, features and capabilities.
There are many options in programming your ICD to treat and interrupt your rapid heart rhythm. Your doctor will program your ICD to deliver the best therapy for you.
Your ICD is part of a system that has two main parts — the ICD and the leads. An external programmer — a small computer that can “talk” to your ICD- remains in your doctor’s office for use during follow-up care.
The ICD continually monitors your heart, watching for any rapid, slow or irregular heart rhythm. When it detects one, it delivers an electrical therapy to return your heart to a more normal rhythm. The ICD is made of titanium metal and contains a battery, a microprocessor (a small computer), and electronic circuitry.
The ICD’s memory stores important information that your doctor retrieves during follow-up visits. The ICD recalls the number and types of treatments you receive, how successful each treatment was in stopping your rapid rhythm, what your heart was doing during your most recent episodes, and the status of the ICD’s batteries and programmed settings.
The leads are insulated wires that are threaded through a vein from the ICD to the inside of your heart. They carry electrical impulses from the ICD to your heart. Since your ICD is always monitoring your heart, the leads also carry information signals from your heart to the ICD. Depending on the type of ICD. you have, one or more leads may be used.
Your doctor and nurse will use the external programmer prior to hospital discharge and during follow-up appointments. The programmer is used to “talk” to your ICD — to make sure it detects and treats your rapid heart rhythm properly. During follow-up visits, it is used to retrieve many useful facts stored in the ICD’s memory. Use of the programmer does not require surgery.
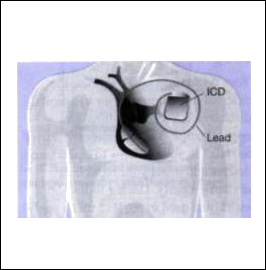
To implant the ICD and leads, your doctor will first decide what type of surgery is needed. He or she will base the decision on your size and shape, whether you have already had chest surgery, and what method is safest for you. Whichever method is used, the ICD will be implanted in your upper chest or under the skin or muscles in your abdominal area.
Before you leave the hospital, your doctor may test the ICD by starting a rapid heart rhythm and having the ICD correct it. This test may also let you know what the therapies might feel like (see What the Treatments May Feel Like).
Potential Complications of this device include failure to detect and/or end tachyarrhythmia episodes, an increase in ventricular tachycardia, and complications involving lead systems.
Because your ICD runs on a battery that is sealed inside it, the ICD will eventually have to be replaced. This procedure is typically easier and quicker than the first implant. How long the ICD lasts depends on the number and types of treatments it delivers.
At replacement time, your doctor will make a new incision over the old one and then remove the old ICD. He or she will then disconnect and check the leads to determine if replacement of the leads is also necessary.
The leads are connected to the new ICD and the ICD’s function is tested. The new ICD is then inserted and the incision is closed. Finally, the ICD is programmed.

Follow-up visits are important to ensure that your ICD continues to work properly. During these visits, your doctor or nurse checks the ICD’s battery status, monitors any medications you are taking, and checks for possible interactions with the ICD. Also, as your condition changes, your doctor may reprogram the ICD to better treat your rapid heart rhythm.
Your doctor or nurse will give you a schedule of regular follow-up visits.
When your ICD detects a rapid heart rhythm, it tries to correct it with therapies programmed by your physician. The ICD can be programmed to deliver therapies that begin mildly and become progressively stronger, as needed. Your ICD can deliver three types of therapy : antitachycardia pacing, cardioversion and defibrillation.
Antitachycardia Pacing : If your VT is relatively slow, your doctor may program the ICD to deliver small, rapid pacing signals when it detects the VT. If the normal rhythm is restored, no further treatment is delivered.
Cardioversion : If pacing does not stop the rapid heart rhythm, the ICD can be programmed to deliver stronger impulses. These cardioversion shocks may be programmed from low energy to high energy, as needed.
Defibrillation : If the ICD detects VF, it will send a high-energy shock to your heart. This defibrillation shock interrupts the rapid heart rhythm so a more normal rhythm can be restored.
If your ICD detects a very slow heart rate (bradycardia), it will pace your heart until it maintains a normal rate. This is called bradycardia pacing.
Many ICDs feature rate responsive pacing. If you are engaged in physical activity such as walking, exercising, or gardening, rate responsive pacing automatically adjusts your pacing rate to match your level of activity. When you slow down, rest, or sleep, the rate decreases accordingly.
As you recover, follow your doctor’s suggestions about resuming normal activities. Expect a gradual recovery. Often, patients say that they are very aware of the ICD in the beginning, but gradually adjust to it.
Because the ICD is a life-saving aid, you may be able to enjoy a wider range of activities.
The First Few Weeks
As you recover from the surgery, follow your doctor’s directions, including :
Exercising, bathing, and walking according to your doctor’s directions.
Avoiding tight clothing that may irritate the skin over the ICD.
Limiting arm movements as directed by your doctor.
Avoiding lifting more than 10-15 pounds.
Avoiding excessive pushing, pulling, or twisting.
Reporting any redness, swelling, or drainage from your incisions.
Telling your other doctors and dentist that you have an ICD. They may need to give you antibiotics before and after surgery or dental work to prevent infection.
Depending on your conditions, your doctor may ask you to avoid situations where a few seconds of unconsciousness due to your rapid hear rhythm could be dangerous to you or others. Such activities may include driving, swimming or boating alone, or climbing a ladder.
You may be able to resume driving, depending on the laws in your area and on your individual condition. Your doctor will decide what is best for your safety and the safety of others.
Upon the advice of your physician, you can gradually return to your normal lifestyle. Such activities might include.
Pursuing hobbies or recreational activities.
Returning to your job.
Resuming strenuous activity.
Resuming sexual activity.
Traveling.
The key to returning to your daily activities is that they should make you feel better, not worse.
Phone your doctor or nurse If you :
Receive a shock from the ICD and have been instructed to call (See What To Do If You Receive A Shock).
Have symptoms of rapid heart rhythm that last longer than three minutes or the length of time specified by your doctor.
Patient Alert tone sounds.
Notice any swelling, warmth, or drainage at any incision.
Develop a fever that does not go away in two or three days.
Have any questions about the ICD or your medications
Plan to travel or move or
Notice anything unusual, such as new unexplained symptoms or symptoms such as those you had before you received the ICD.
Things that use magnets and electricity have electromagnetic fields around them. These fields are usually weak and will not affect your ICD. However, strong electromagnetic fields can interfere with your ICD. This is called EMI or electromagnetic interference. A strong electromagnetic field can temporarily “blind” your ICD, preventing it from treating you or causing an inappropriate delivery of a shock.
It is important to know which sources of EMI do and do not affect your ICD. A discussion of the common sources of EMI follows.
Operating Household Appliances and Tools
The ICD’s built-in features protect it from most interference produced by electrical appliances. You can operate most household appliances and tools that are in good repair, including :
Microwave ovens
Televisions, AM/FM radios, VCRs, remote controls
Garage door openers
Tabletop appliances; toasters, blenders, electric can openers, electric knives, etc.
Hand-held appliances: hair dryers, shavers, etc. (avoid holding against your implant site).
Major appliances: washers, dryers, electric stoves, refrigerators, etc.
Electric blankets and heating pads
Spark-ignited internal combustion engines: lawn mowers, leaf blowers, automobiles, etc.
You can also operate the following office and light shop equipment that is properly grounded and in good repair:
Personal computers, printers, electric typewriters, fax machines, copying machines
Machine shop equipment: drills, table saws, etc. (keep tools 12 inches from implant site)
Things to Avoid
To ensure proper function of your ICD, you should avoid the following :
Industrial equipment
Arc and resistance welders
Induction furnaces
Large generators and power plants
Large magnets, such as those used in some stereo speakers, bingo wands, extractor wands, magnetic badges and magnetic therapy products
Antennas used to operate a CB, ham radio, or other radio transmitters including those used to control toys
Large TV or radio transmitting towers and power lines carrying more than 100,000 volts (maintain a distance of 25 feet between you and the towers or lines)
Possible hidden sources of electromagnetic energy
Maintenance or repair of any electrical or gas-powered appliance or tool
Other tools, such as chain saws, that can cause harm if you become dizzy or receive a shock while operating
Touching the spark plug or distributor on a running car or lawn mower. Turn the engine off.
If you have questions about any situation or piece of equipment, contact your doctor or nurse.
Always tell any medical personnel that you have an ICD. With proper precautionary measures, most medical procedures are unlikely to interfere with your ICD. These include:
Diagnostic X-rays: chest X-rays, dental X-rays, CT scans, and mammography. Mammograms require a tight enclosure of the chest by X-ray equipment. If you have an upper chest implant, adjustments that lessen pressure are sometimes used to make the patient more comfortable.
Dental procedures, including the use of dental drills and ultrasonic probes used to clean teeth.
Therapeutic ultrasound, TENS, and electrolysis may be used with proper precautions — providing the equipment is not placed directly over the implant site.
Other medical procedures produce high levels of interference. You may wish to discuss with your doctor or nurse the risks and benefits of procedures such as electrosurgery, diathermy, lithotripsy, and radiation therapy.
Magnetic resonance imaging (MRI) is not recommended for ICD patients at this time. If use of an external transthoracic defibrillator is needed, do not place paddles directly over device.
Always tell medical personnel that you have an ICD.

It is okay to walk through security screening archways, such as those at airports and government buildings. The archway may detect your ICD’s metal case and set off the alarm. However, your ICD will continue to function normally. If the alarm sounds, present your ICD identification card to security personnel and ask that they clear you after only a hand search – without a hand-held screening wand. Any repetitive motions of a hand-held screening wand may temporarily interfere with the proper operation of your ICD. This is because the wand has a strong magnet in it.
At the entrance to stores, libraries, etc., walk normally through theft detector systems. Do not stop in areas adjacent to the detection equipment.
Using Cellular Phones
As a new ICD recipient, you do not need to take any special precautions when using cellular phones. The ICD you have just received has been tested to the frequency ranges used by the cellular phones included in the table on the next page.
The circuitry of this device allows usage, without interaction, of all cellular phones having one of the transmission technologies listed on the table on page. These transmission technologies represent the vast majority of cellular phones in use worldwide.
You and your doctor can contact your local cellular phone service provider to confirm that the provider uses one of these technologies.

If you feel the symptoms that tell you your rapid heart rhythm has begun :
Follow your doctor’s or nurse’s directions on when to call them after receiving a shock. When you call, you may be asked:
• What were you doing right before the shock?
• What symptoms did you notice before the shock?
• How did you feel right after the shock?
Stay calm and move to where you can lie down or sit comfortably.
Have someone stay with you throughout the event, if possible.
Have a friend or family member prepared to phone for an ambulance if you receive shocks and remain unconscious for more that a minute.
If you do not feel well after the shock, have someone call your doctor and help you prepare to be taken to the emergency room of the nearest hospital.
Anyone touching you while the ICD delivers a therapy shock might feel the muscles or your chest and upper arms contract and might see you jump as. though startled. The shock will not harm the person touching you.
It is a good idea to have an emergency plan. There is space in the front of this booklet for local emergency medical phone numbers and information about your current medications. Keep this information near your phone.
Give yourself and your family a few months to adjust to living with your ICD. Most people develop a positive attitude toward the ICD. At times, some patients say they feel depressed, anxious, vulnerable, angry, or afraid. If these feelings last for more than a couple months, talk to your doctor or nurse about seeking advice from someone who is qualified to give you suggestions.
You may also want to speak to other patients who have received an ICD and ask them how their families have adjusted to the ICD. Ask your doctor or nurse if there is a support group of ICD patients at the hospital.
With time, your confidence will return as you resume work, activities, and family life.
Your family can be a big support for you during your hospitalization. Encourage them to learn about your ICD and about how they can continue to support you at home. If they have any questions or concerns, have them call your doctor or nurse.
Some friends and family members may want to receive training in cardiopulmonary resuscitation (CPR). They also may want to attend support group meetings with you.
Travel
With your doctor’s permission, you will be free to travel with the ICD. When you plan a trip, remember to :
Contact your doctor or nurse for instructions. Ask for the name of a physician or heart center in the state or country you are visiting.
Show your ID card to airport security and ask for a hand search without a hand-held screening wand.
Arrange with your doctor to see another physician if you will be away for more than three months.